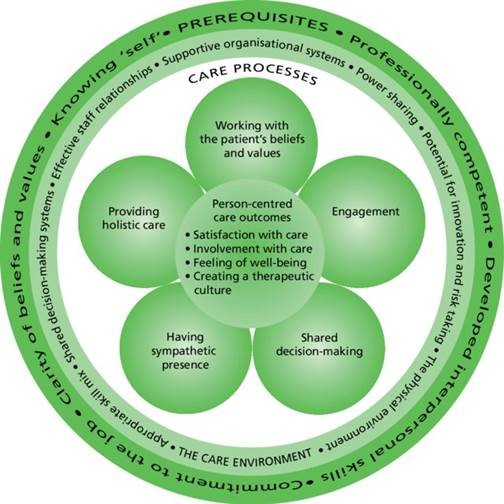
“Health care that is personalized and tailored to patient values”
The overall vision for people-centred health care is one in which individuals, families and communities are served by and are able to participate in trusted health systems that respond to their needs in humane and holistic ways. The health system is designed around stakeholder needs and enables individuals, families and communities to collaborate with health practitioners and health care organizations in the public, private and not-for-profit health and related sectors in driving improvements in the quality and responsiveness of health care.
People-centred health care is rooted in universally held values and principles which are enshrined in international law, such as human rights and dignity, nondiscrimination, participation and empowerment, access and equity, and a partnership of equals. It aims to achieve better outcomes for individuals, families, communities, health practitioners, health care organizations and health systems by promoting the following:
- Culture of care and communication. Health care users being informed and involved in decision-making and having choices; providers showing respect for their privacy and dignity and responding to their needs in a holistic manner.
- Responsible, responsive and accountable services and institutions. Providing affordable, accessible, safe, ethical, effective, evidence-based and holistic health care.
- Supportive health care environments. Putting in place appropriate policies and interventions, positive care and work environments, strong primary care workforce, and mechanisms for stakeholders’ involvement in health services planning, policy development and feedback for quality improvement.
The major challenge confronting health systems is the need to tip the balance away from health services that are overly biomedical oriented, disease focused, technology driven and doctor dominated. There is a clear call to restore balance in health care and the health system itself.
Individuals, families and communities
Holistic and compassionate health care requires an effective partnership between people who need care and people who provide care. To achieve this, action is required to support capacity-building for better informed and more empowered individuals, families and communities who are able to actively participate in health care and in health systems development. Strategic responses could include:
(a) Increasing health literacy
- community and mass media education campaigns;
- skills-oriented health education programmes in schools;
- written information in conjunction with verbal information in clinical consultations; and evidence-based health education through the web.
(b) Providing communication and negotiation skills that lead to meaningful participation in decision-making
- personalized and comprehensive decision-making aids, including computer-based and web-based health education packages; and
- access to health records, including audio recordings and written summaries of clinical consultations, as appropriate.
(c) Improving capacity for self-management and self-care chronic disease management training programmes;
- computer or web-based targeted health education programmes;
- referral to appropriate patient or peer support groups; and
- interventions that promote patient adherence to medication regimes, e.g. providing explicit written instructions about taking prescribed medicines.
(d) Developing community leaders who advocate and support community involvement in health service delivery
- identification of suitable leaders in local communities;
- leadership development programmes; and
- mechanisms for participation in hospital boards, health care advisory
Health Practitioners
Competent health practitioners are required to deliver health care that is responsive to the needs, preferences and expectations of people accessing health services. The most effective and appropriate intervention in this domain is appropriate education and training of health practitioners. Strategic responses could include:
(a) Increasing capacity for holistic and compassionate care
- identification of core competencies of people-centred health practitioners;
- promotion and integration of core competencies in all education and training programmes for health practitioners; and
- development of comprehensive, harmonized medical, nursing and allied health community-based training that:
- are skills-oriented;
- emphasize bio-psychosocial and spiritual factors;
- include humanities-based subjects (such as medical ethics) in addition to the clinically oriented subjects;
- cover communication skills, building trust and developing tailor-made interventions;
- increase cultural competency;
- facilitate understanding of psychosocial dimensions of health and illness and of the role of traditional medicine in health care;
- promote evidence-based practice;
- feature a balance of family medicine and specialties;
- develop skills necessary for working in a multidisciplinary team;
- inculcate a culture of reflective practice;
- encourage life-long learning, personal growth and development;
- instill the importance of taking care of one’s health and wellbeing;
- utilize a variety of teaching and learning strategies; and
- provide continuing professional development for health practitioners in a number of forms (i.e. Internet, professional associations and journals).
b) Enhancing commitment to quality, safe and ethical services
- formation and reinforcement of people-centred values in continuing education, professional codes of conduct, and workforce development and regulation policies; and
- recognition of and support for clinical educators and role models who espouse professionalism and humanism in health care and transfer values to trainees through active modes of instruction.